
Number of patients with a final diagnosis of ischaemic stroke, with documented atrial fibrillation, separated from hospital.Īustralian Commission on Safety and Quality in Health Careįurie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC et al. Number of patients with a final diagnosis of ischaemic stroke with documented atrial fibrillation who were prescribed oral anticoagulation therapy on separation from hospital. advance care directive is enacted and/or the patient is on a palliative care pathway). where there are limitations of therapy (i.e.

The numerator requires evidence of prescription of oral anticoagulation therapy at the point of the patient being separated from hospital. Oral anticoagulants include warfarin, apixaban, rivaroxaban or dabigatran.īoth the numerator and the denominator exclude patients for whom oral anticoagulants are contraindicated (where the contraindication is clearly documented). Contraindications may include:
The diagnosis of atrial fibrillation is in addition to the diagnosis of ischaemic stroke.
#TYPE II ATRIAL FLUTTER ICD 10 CODE#
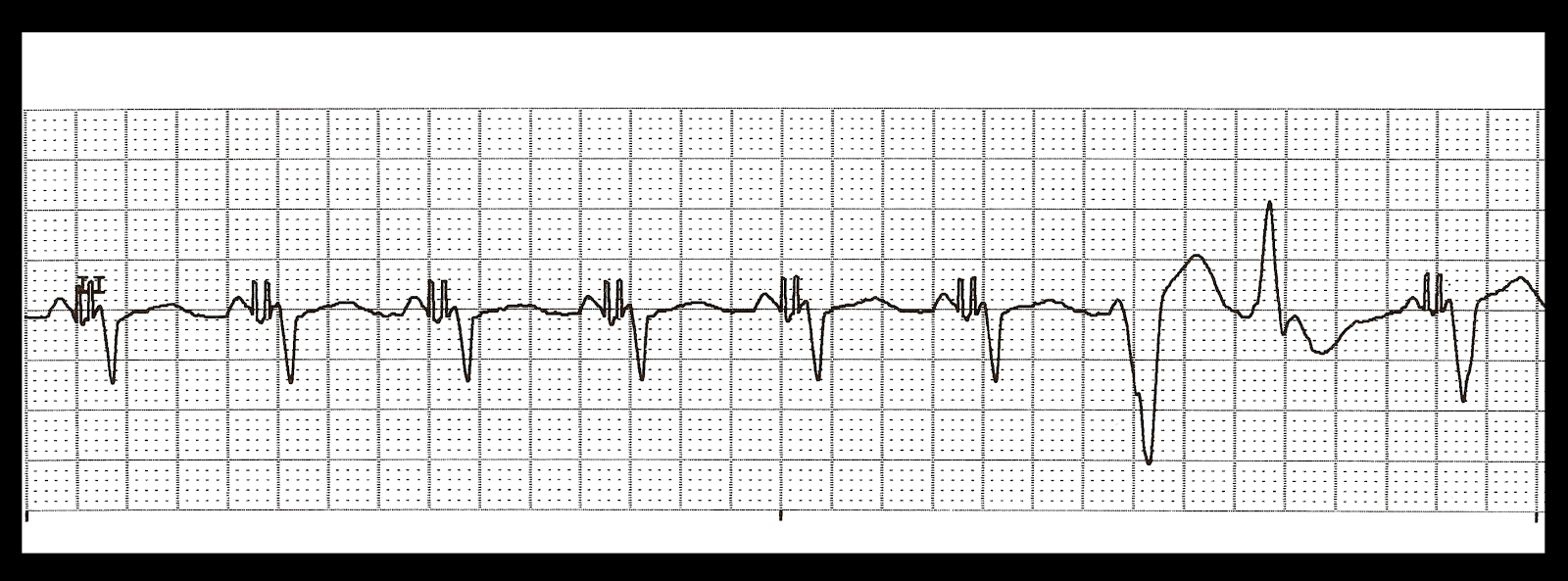
2011).Ĭlinical care standard indicators: acute strokeīoth the numerator and the denominator include patients with a final diagnosis of ischaemic stroke and atrial fibrillation.Ītrial fibrillation includes patients where Episode of care-principal diagnosis, code (ICD-10-AM 9th edn) ANN is one of the following: The administration of oral anticoagulation therapy, unless there are contraindications, is an established effective strategy in preventing recurrent stroke in patients with a high stroke risk, such as those with atrial fibrillation, or prior transient ischaemic attack (TIA) or stroke (Furie et al. Non-valvular atrial fibrillation is a common arrhythmia and an important risk factor for stroke. Proportion of ischaemic stroke patients with atrial fibrillation prescribed oral anticoagulants, where not contraindicated, on separation from hospital. Indicator 5c-Oral anticoagulants prescribed for atrial fibrillation on separation from hospital In conclusion, radiofrequency catheter modification or ablation of the AVN for rapid AF and ablation for atrial flutter type I are demonstrated to be highly effective in the majority of ICD patients with drug refractory multiple inappropriate ICD therapies.Acute stroke clinical care standard indicators: 5c-Oral anticoagulants prescribed for atrial fibrillation on separation from hospital Identifying and definitional attributes There was an overall mean incidence of 18 +/- 22 inappropriate ICD therapies per 6 months before and 4 +/- 9 per 6 months after the ablation procedure (P < 0.05). None of the atrial flutter patients had recurrences of inappropriate therapies for type I atrial flutter during 14 +/- 8 months, but two (33%) patients had inappropriate ICD therapies for type II atrial flutter or rapid AF. Three (25%) AF patients had 11 +/- 24 recurrences of ATP and 0.4 +/- 1.1 shock therapies for rapid AF during 15 +/- 7 months. A complete TA-IVC isthmus block was achieved in 5 (83%) of 6 atrial flutter patients. Modification of the AVN was successful in 10 (83%) of 12 AF patients, in 2 (17%) patients ablation of the AVN was performed. Twelve patients received a mean of 34 +/- 36 antitachycardia pacing (ATP) and 41 +/- 32 shock therapies for rapid AF during 49 +/- 39 months, and 6 patients a mean of 111 +/- 200 ATP and 11 +/- 8 shock therapies for type I atrial flutter during 52 +/- 37 months preceding ablation procedure. Eighteen consecutive patients were enrolled in this study. The purpose of this prospective study was to determine the usefulness of AVN modulation or ablation for rapid AF and ablation of the tricuspid annulus-inferior vena cava (TA-IVC) isthmus for type I atrial flutter in ICD patients with frequent inappropriate ICD interventions. Most of the inappropriate therapies for supraventricular tachycardia are caused by AF and type I atrial flutter with rapid ventricular response.
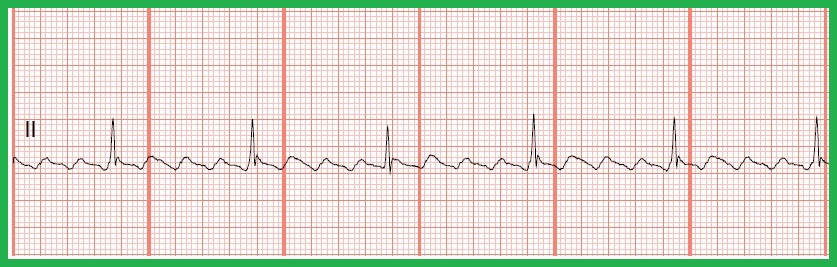
The high incidence of inappropriate therapies due to drug refractory supraventricular tachycardia remains a major unsolved problem of the ICD.


 0 kommentar(er)
0 kommentar(er)
